Catena is now Pearl Talent! Same mission, new name.
You’re not losing money because your care isn’t great. It’s because the admin side of care (the paperwork, coding, insurance follow-ups) is bogging your team down. Billing delays, rejected claims, and authorization misses often start long before they even reach the billing desk. These issues not only affect reimbursement but can ripple into patient satisfaction, operational efficiency, and financial stability.
This is where healthcare revenue cycle management (RCM) can make or break a practice. When your front-end admin processes are scattered, you pay for it on the back end through cash flow gaps, denied claims, and burnout across your team.
At Pearl Talent, we help fix those pain points by placing experienced, fully-managed RCM professionals into the specific parts of your workflow where things fall through: eligibility checks, pre-auths, coding, submissions, and denial follow-up. No generalists. No guesswork.
In this article, you’ll get a practical breakdown of what healthcare revenue cycle management really involves. We’ll walk through the key steps that affect your ability to get paid, where most practices lose money without realizing it, and what kind of support can finally stop the cycle of delays, denials, and endless rework.
What Is Healthcare Revenue Cycle Management (RCM)?
Healthcare revenue cycle management is the end-to-end process healthcare providers use to track, manage, and collect revenue, from the moment a patient books an appointment to the final payment of their balance.
When most people think of medical billing, they think of the final invoice. But by then, it’s too late. RCM starts much earlier and goes much deeper. It connects every administrative and clinical action that influences how, and whether, a provider gets paid.
Put simply, RCM is the financial backbone of your practice. It includes scheduling, insurance verification, coding, billing, denial follow-up, and more.
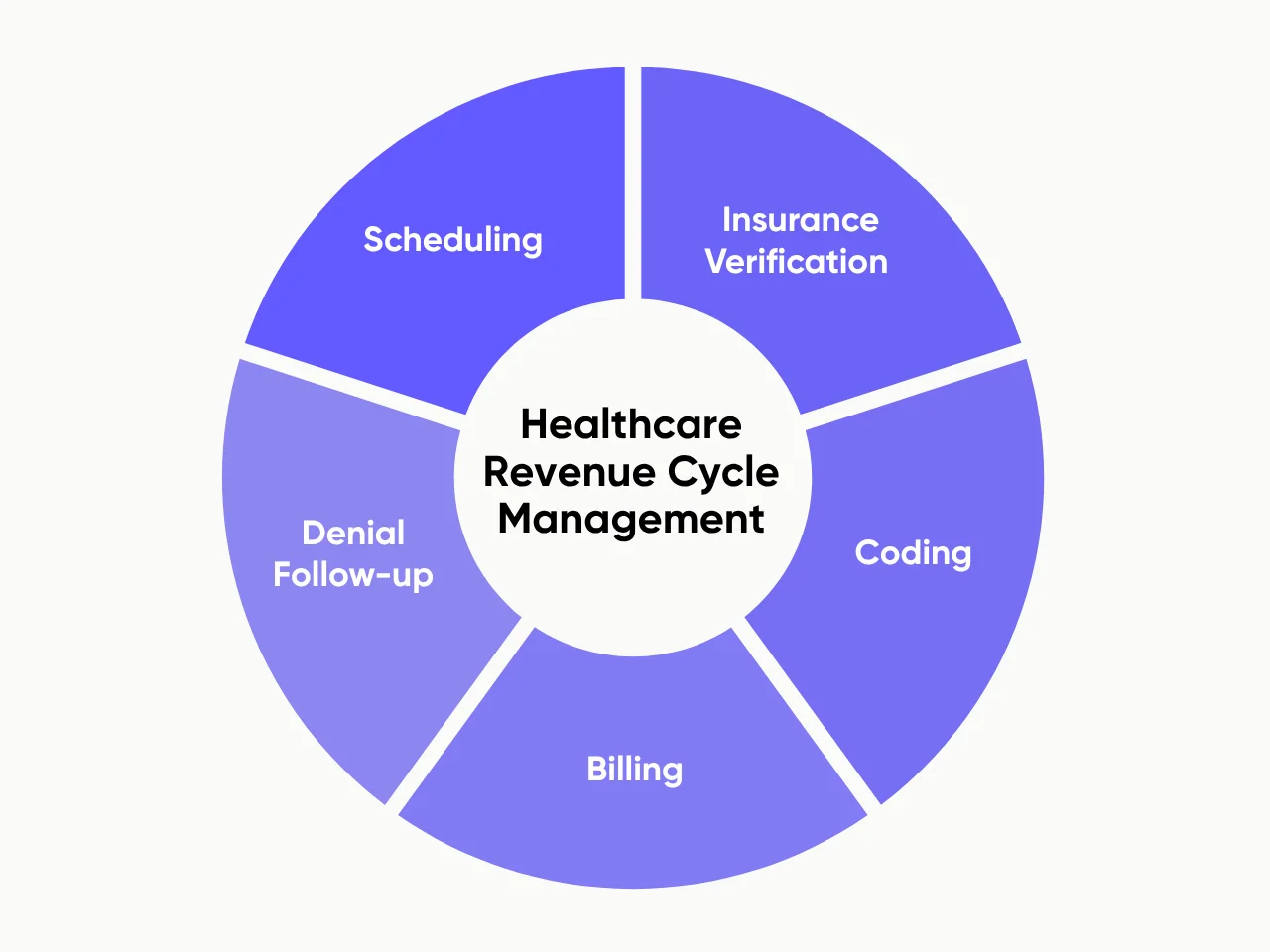
If even one of these steps fails, the whole system slows down or breaks.
Think of it like tracking a package. You don’t just send it and hope it arrives. You scan it at every step: pickup, sorting, transport, delivery. A missed scan delays the delivery or sends it to the wrong place. In healthcare, that “missed scan” might be an unchecked insurance ID, an incomplete authorization, or a miscoded procedure, all of which delay or kill reimbursement.
RCM isn’t just “admin work.” It’s how you make sure the care you provide actually results in payment. Like any system, it only works if every step is owned, tracked, and executed in a timely manner.
The 7 Basic Steps of the Healthcare Revenue Cycle
Revenue issues don’t usually stem from one major mistake. They come from small oversights compounding over time. The healthcare revenue cycle is a chain of interconnected steps that moves a patient from their initial appointment to full reimbursement. And when even one step is rushed, skipped, or handled by the wrong person, claims stall, denials rise, and revenue slips through.
Let’s walk through each step, what it looks like in practice, and where breakdowns commonly occur.
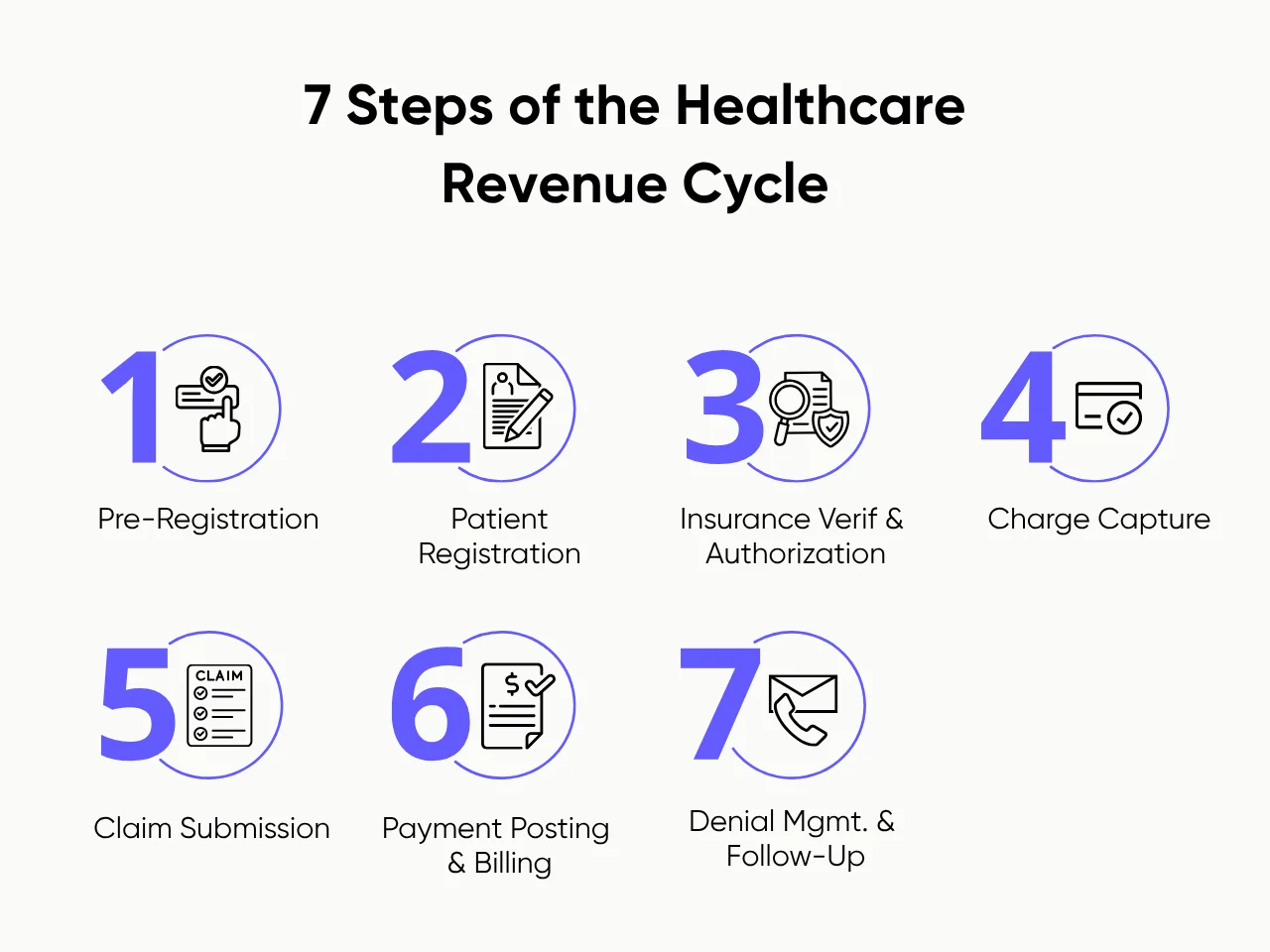
1. Pre-Registration
This is where everything starts: during scheduling. Your team collects the patient’s insurance details, confirms plan status, and flags services that require prior authorization. When done well, it prevents:
- Denied claims due to inactive or expired insurance coverage
- Delayed care caused by missing referrals or prior auths
- Front desk scramble when key details weren’t gathered in advance
When the front desk is juggling phones, walk-ins, and follow-ups, pre-registration becomes a “when we can” task. But this step is too critical to multitask. That’s why many practices now assign a dedicated pre-reg role, often remotely, to keep this part of the process airtight.
2. Patient Registration
This happens at check-in. It’s where the front desk confirms demographic data, insurance ID numbers, and contact information, and corrects anything that’s changed since pre-reg. Here’s why this matters:
- Even a small human error can cause a mismatch that leads to a claim denial.
- Outdated info can delay billing and frustrate patients with inaccurate statements.
- Correct records help billing teams avoid unnecessary backtracking or rework.
For example, a patient changes jobs and their insurance plan changes. If your front desk doesn’t catch that at check-in, your team may unknowingly bill the wrong payer, which could result in a rejection that takes weeks to clean up.
3. Insurance Verification & Authorization
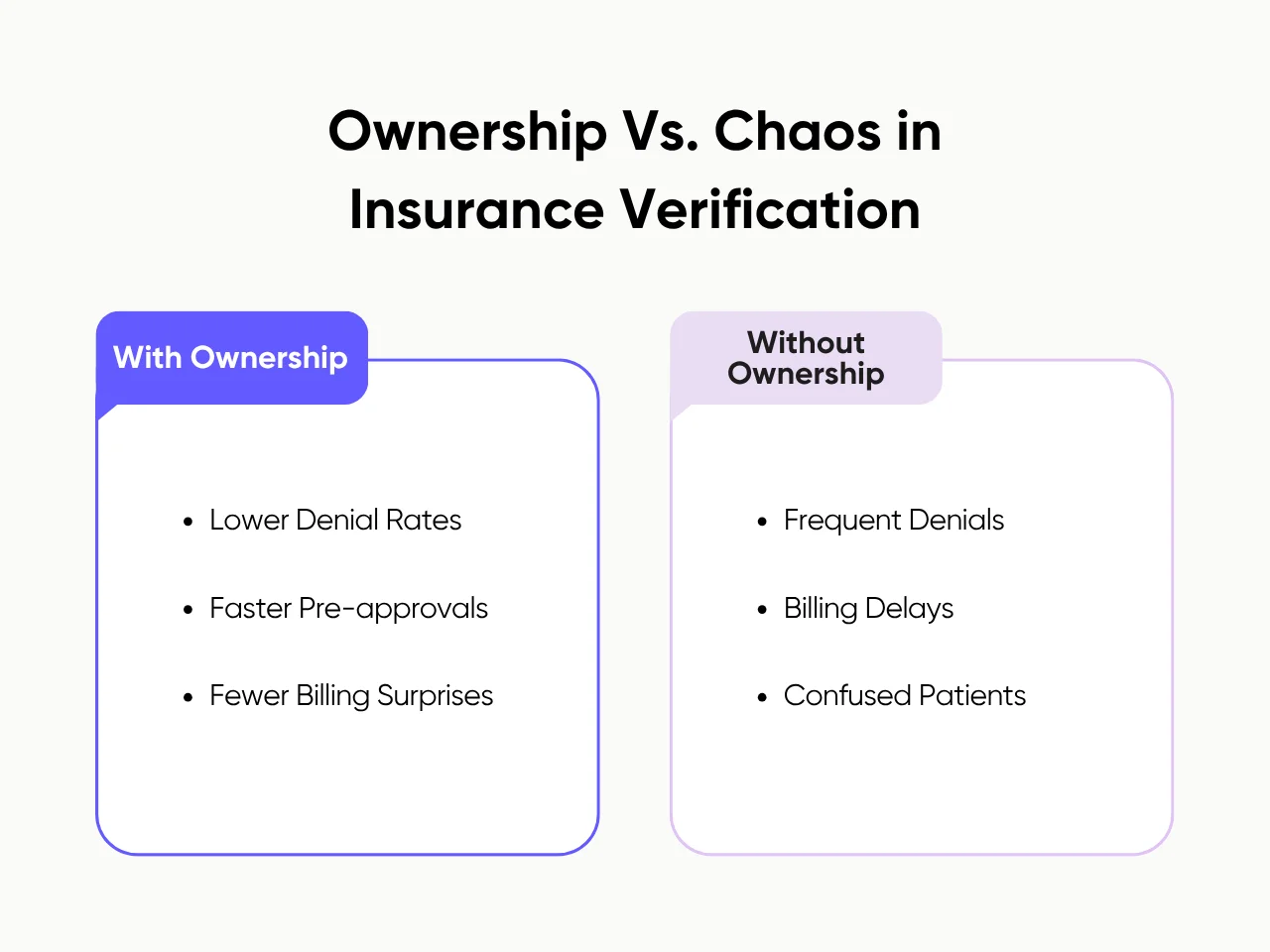
This step confirms the patient’s benefits are active and that any needed authorizations are secured before the visit. It’s not just an admin formality. It’s a revenue safeguard. And when it’s done correctly, it helps you:
- Avoid denials for services that require pre-approval
- Catch inactive plans or authorization expiration before the visit
- Spare patients the shock of a bill for a service they thought was covered
Many practices rely on staff to juggle verification between other duties. But when no one’s truly owning it, things fall through. That’s why more healthcare teams are turning to dedicated RCM specialists, like the ones we provide at Pearl Talent, to take ownership of this step and reduce denials from the start.
4. Charge Capture
This is the handoff from care to billing. After the appointment, services must be documented and coded (e.g., CPT, ICD-10) for billing. Basically, charge capture ensures:
- Every billable service is properly documented and coded according to current industry standards
- Revenue isn’t lost due to under-coding or vague documentation
- Claims are defensible if ever audited or challenged
A common issue this step can resolve is when documentation is unclear or vague. Coders can’t bill confidently, which often leads to underbilling to avoid risk. That’s revenue left on the table.
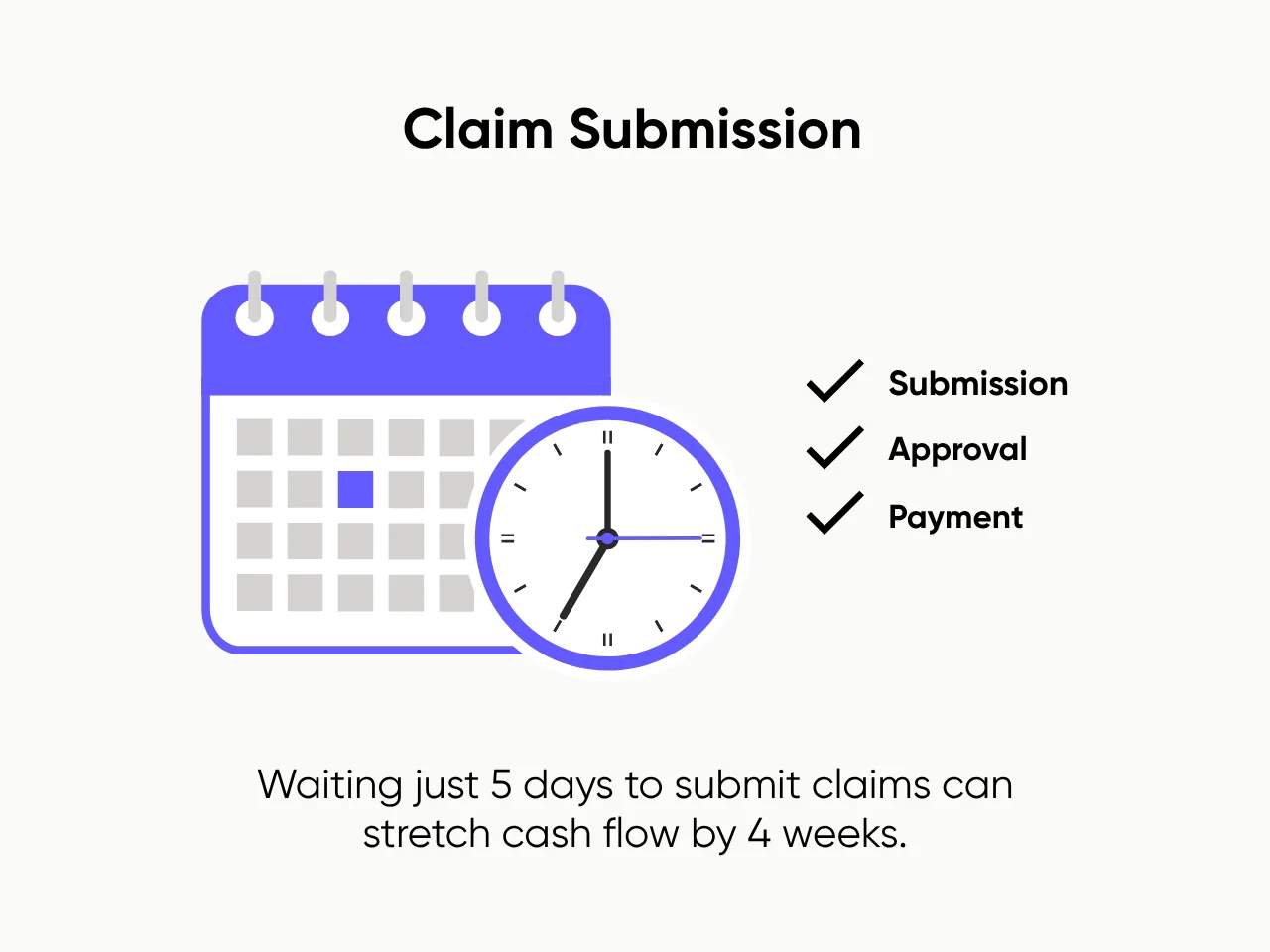
5. Claim Submission
Once codes are applied, your team builds the claim and submits it to the insurance payer. This stage hinges on speed, accuracy, and payer-specific compliance. Strong processes here mean:
- Clean claims get submitted and accepted faster
- You don’t miss deadlines due to batching or backlogs
- Your accounts receivable (A/R) stays lean and predictable
Many smaller practices still submit claims in weekly batches. That delay alone can stretch cash flow by weeks.
6. Payment Posting & Patient Billing
This is where received payments are posted to the correct accounts, and patient statements (including co-pays and deductibles) are sent out. Accurate posting ensures:
- Your books reflect the true financial picture
- Patients get clear, correct bills, reducing confusion and complaints
- Your team can prioritize real collections, not spend time untangling misapplied payments
7. Denial Management & Follow-Up
Claims don’t always get paid the first time. This is where the cleanup needs to happen, which involves resolving denials, underpayments, or no responses. And when done consistently, denial management can:
- Recover significant revenue that would otherwise be written off
- Surface patterns (for example: one provider’s coding, one payer’s quirks) to fix upstream
- Shorten A/R cycles and boosts overall financial health
We've seen practices lose five to six figures per year from denials no one had time to chase.
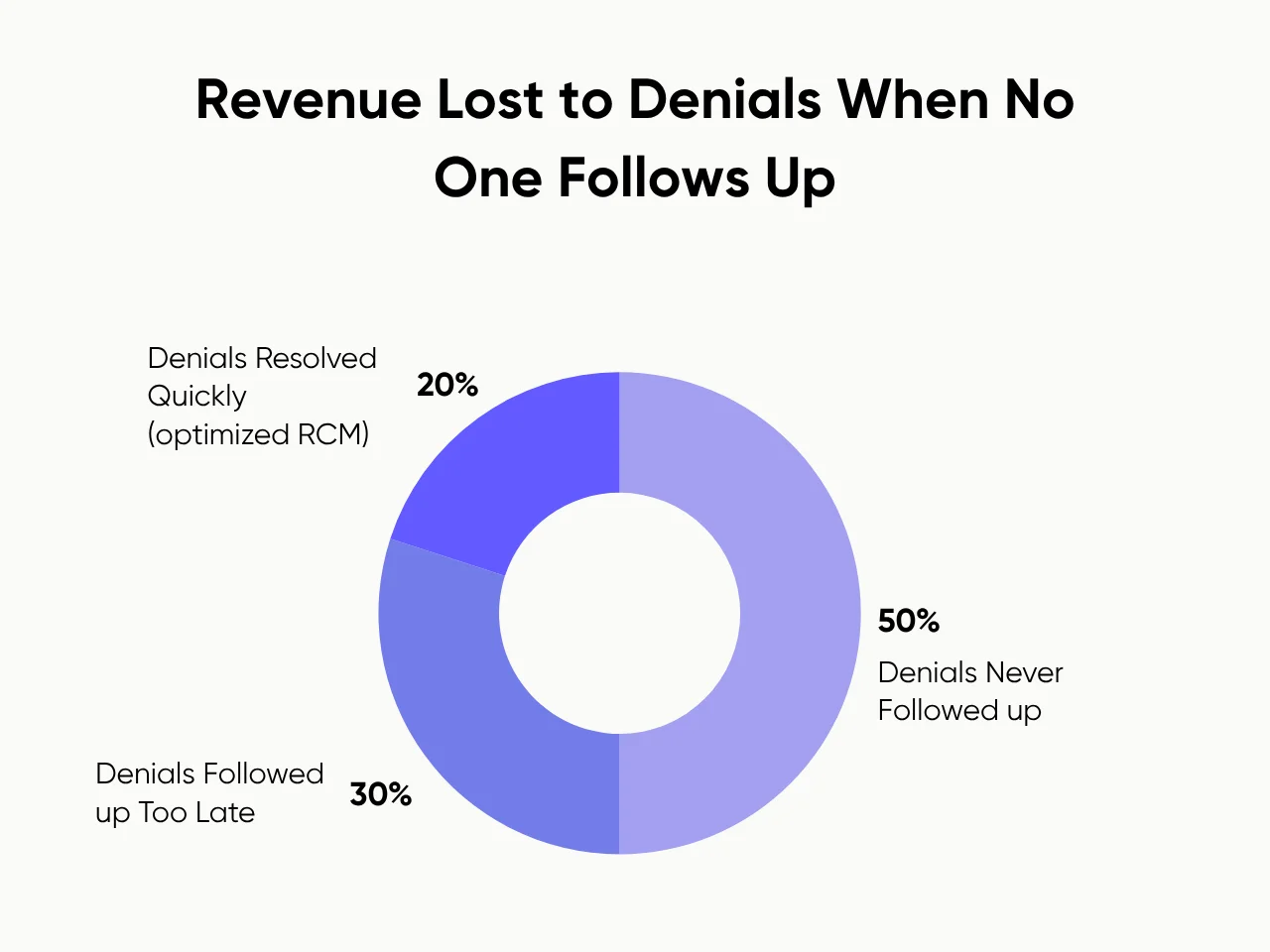
Having dedicated RCM support, even part-time, can make a measurable difference. At Pearl Talent, we plug in experienced specialists where they're needed most, so your internal team isn’t left scrambling to recover missed revenue.
Why RCM Matters for Small and Mid-Sized Practices
In small and mid-sized healthcare practices, problems in the revenue cycle often manifest as dozens of minor issues: a missed pre-authorization, a late claim, or a denial that goes unnoticed. While each on its own feels manageable, they can compound into cash flow headaches, overworked teams, and a billing process that feels reactive rather than reliable.
Let’s break down how better revenue cycle management improves the core areas that matter most to growing practices: payment speed, team capacity, and scalability.
Faster Payments Mean Smarter Decisions
When revenue is slow or unpredictable, everything from hiring to supplies to payroll becomes a guessing game. With healthcare costs in the United States continuing to rise, it’s even more critical to keep your revenue predictable. Clean revenue cycle management in medical billing keeps reimbursement timelines tight and cash flow consistent.
With the right system and support in place:
- Claims go out daily, not in batches, which accelerates payment cycles
- Denials are resolved quickly, not pushed off until someone has time
- Follow-ups happen proactively, so money doesn’t sit in limbo for weeks
For practices running lean, faster revenue isn’t just convenient; it’s survival. Steady reimbursement lets you make growth decisions based on actual performance, not credit or gut feel.
It Keeps Your Team Focused (and Sane)
Most smaller practices don’t have a dedicated RCM department. Instead, billing and insurance tasks are scattered across whoever has capacity: front desk staff, part-time admins, and even medical assistants. That leads to:
- Multitasking critical steps, like authorizations or charge entry
- Inconsistent workflows that rely on memory or habit, not process
- Burnout, especially when visit volume spikes or team members leave
Better RCM gives every task an owner, and that owner doesn’t have to be on-site.
At Pearl Talent, we place trained RCM professionals into your workflow to take ownership of high-leverage steps like eligibility checks, claim submission, or denial follow-up. They’re managed, supported, and performance-tracked so your internal team doesn’t have to carry everything.
It Makes Growth Sustainable
When patient volume increases, your systems get stress-tested. And if your RCM is already duct-taped together, growth won’t help. It’ll just expose the cracks faster.
With a structured revenue cycle process in place:
- You gain capacity without overhiring or burning out your team
- Your billing operation scales with patient volume, not against it
- You stop throwing people at the problem and start building a process that lasts
Waiting until things are broken to fix your RCM is like waiting for your A/R to hit six figures before investigating your claim queue. Practices that implement structured support early often avoid the worst pain points altogether.
At Pearl Talent, we work with scaling practices to build that support system from day one. We help you plug in fully-managed RCM talent exactly where your current process is weakest, whether that’s at intake, billing, or back-end follow-up. This way, your team can keep moving without falling behind.
Common RCM Challenges and Mistakes
Even if your practice has the right tools and intentions, revenue problems still happen. Not because you’re doing nothing, but because critical steps in the process aren't clearly owned or consistently executed. Most billing breakdowns aren’t obvious until the end of the month (or quarter).
Here are five of the most common mistakes we see in revenue cycle management healthcare settings, and what they look like when they happen inside small and mid-sized practices:

Incomplete Patient Data
It starts at intake. One missing insurance group number, an outdated plan, or an unverified Social Security Number, and suddenly, you’ve got a denial two weeks later that takes another two weeks to fix.
Here’s an example: A patient updates their insurance with the front desk but forgets to mention that the new plan requires referrals. The claim gets denied, and your team spends hours tracking the patient down, gathering new paperwork, and resubmitting, and that’s for a visit that already happened.
Delayed Claim Submissions
Many practices still send out claims once a week (or less), especially if billing is just one of many tasks someone owns. But those delays, even without errors, can drag out cash flow by 20 to 30+ days.
And the impact? Slow claim cycles don’t just delay payment. They shorten your window to correct or appeal denials. The longer you wait to submit, the less room you have to fix mistakes before deadlines hit.
Poor Denial Follow-Up
Denied claims don’t disappear on their own. But without a clear owner watching the queue, most of them get deprioritized or written off. Poor follow-ups lead to missed revenue.
Lack of Billing Expertise In-House
When billing tasks are handed to generalist staff, such as medical assistants or receptionists, problems do not result from a lack of effort. Instead, they result from a lack of training in RCM-specific details: coding logic, payer rules, modifier use, and timely filing limits.
Billing, then, becomes a guessing game. Staff err on the side of underbilling to avoid denials, or they submit incomplete claims that create work downstream. Either way, revenue suffers.
No Clear Ownership of the Billing Process
This is the silent killer. Everyone assumes someone else is watching the numbers. But when ownership is scattered, tasks slip, and no one notices until A/R balloons or payments stop coming in. So, here’s what to look for:
- Are claims consistently submitted same-day?
- Is someone regularly reviewing and working the denial queue?
- Do you know which staffer owns which part of your RCM?
If the answer to any of those is unclear, your revenue is probably leaking, and your team is probably exhausted from constantly reacting instead of working proactively.
Pearl Talent can help close these gaps. We place remote RCM professionals directly into the weak links of your revenue cycle, from intake to billing to follow-up. They're trained, monitored, and equipped to own the work so your internal team doesn’t have to triage problems every day.
Key Takeaway
If your cash flow is inconsistent, your A/R keeps growing, or your team is constantly reacting to denials and delays, your process needs to be optimized. Effective healthcare revenue cycle management ensures that you receive payment for the care you deliver, especially when every step is handled accurately, consistently, and by the right people.
At Pearl Talent, we’ve helped fast-growing healthcare teams reduce claim denials, speed up payments, and finally get control of their billing operations, without having to build an in-house billing team from scratch. Talk to us today!
Frequently Asked Questions
Originally Published
June 5, 2025




.svg)